Is one better than the other? Are they interchangeable? How do they interact? Is a multiple approach the answer? As with anything to do with biology, the answer is “it’s complex”.
Statins have been one of the most prescribed drugs to lower high cholesterol in the US since their introduction in the early 1990s. Let’s start with understanding cholesterol , why should it be lower in many people, and ways to approach it.
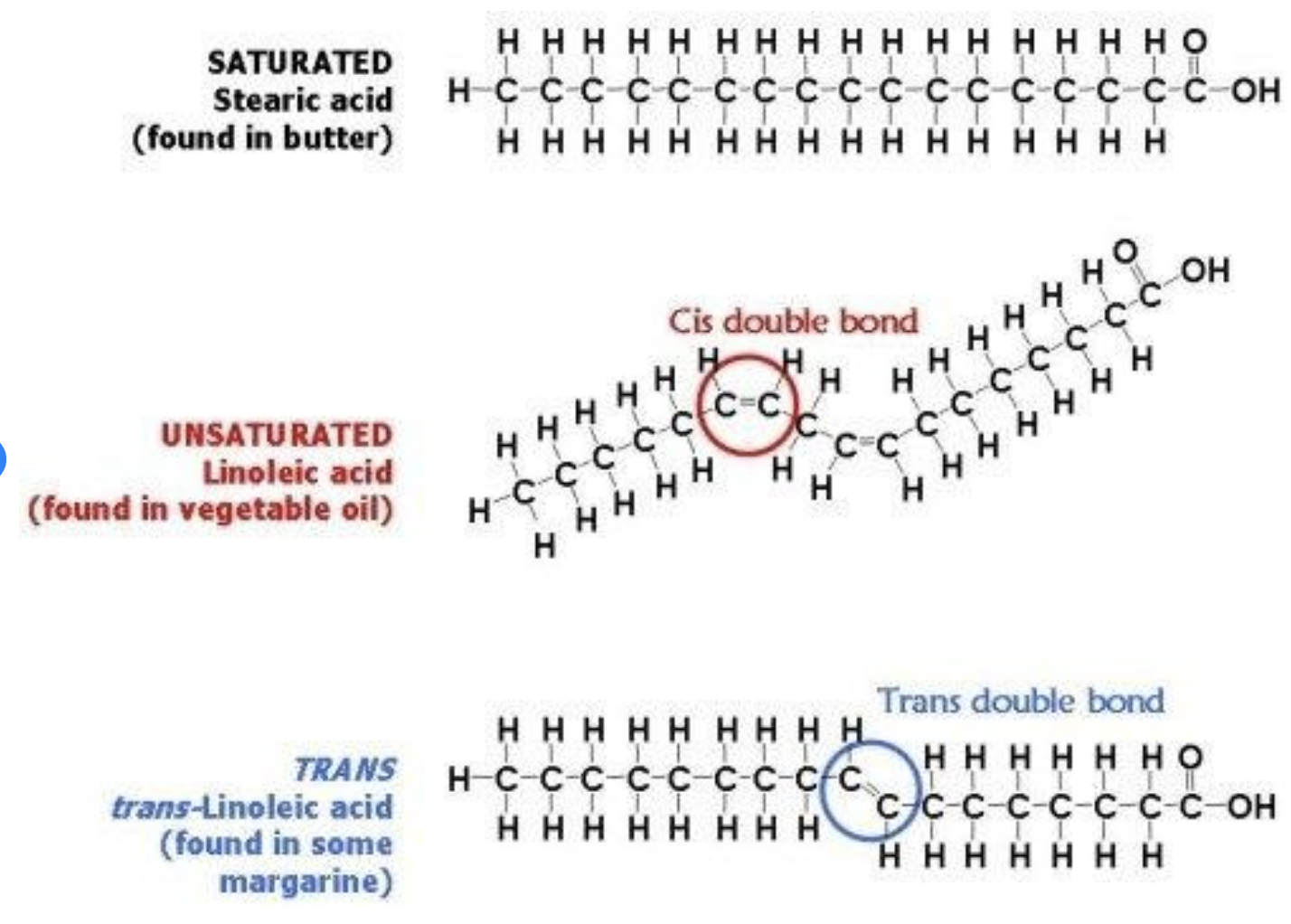
Our livers make a daily genetically-determined amount of cholesterol. It is necessary as a cell membrane stabilizer, a precursor of sex hormones, vitamin D and bile, and as part of the fatty-acid transport system in our blood. Animal foods add a dietary source of cholesterol, but whether dietary cholesterol is actually worrisome has been debated for years (current thoughts -> less problematic, but stay tuned...) We manage cholesterol levels internally with a recycling mechanism that recaptures some, and we also lose some through our gut. The liver uses cholesterol to create bile acids which are secreted into the intestine to facilitate absorption of dietary fats. Some of these bile acids are lost in the feces.
Handy food tips: eating high fiber foods causes more bile to be swept out of the intestine, indirectly lowering your cholesterol. Certain plant foods, (avocado, flax, peanuts) contain phytosterols, which compete with cholesterol for reabsorption sites in the intestine, thus increasing cholesterol elimination. Take home tip: eat higher fiber foods like apples, oats, beans, lentils, leafy greens and consider including avocado, flax and peanuts.
It gets a bit more complicated because you’ll hear about more than one type of cholesterol (total cholesterol reflects the sum of LDL and HDL in lipid profile blood work). Vastly simplified, LDL is a blood-borne vehicle which carries lipids and cholesterol (sloppily) out to the perifery for use in cellular metabolism and repair. The HDL vehicle returns to the liver picking up scraps of cholesterol stuck to the insides of blood vessel walls on the way. Higher HDL levels are good, because it correlates with decreased heart disease risk (you’ll want it high, remember H for high HDL). If one’s levels of LDL creeps up, this is concerning because more cholesterol and fatty acids could get dropped in the blood vessels. Narrowing and hardening of arteries due to plaques, drive up blood pressure and risk of atherosclerotic events such as heart attack and stroke. (So you want it low: remember L for low LDL). Make sure that you know your ratio of HDL to LDL (different for men vs women, but around 3.5 is good). Total cholesterol is a less precise number.
There are a number of tactics to decrease risk of atherosclerosis and improve one’s health span. The simplest one is to go on statins, also known by the following terms: atorvastatin (Lipitor), fluvastatin (Lescol XL), lovastatin (Altoprev), pitavastatin (Livalo), pravastatin, rosuvastatin (Crestor) and simvastatin (Zocor). Statins are a class of pharmaceuticals that block the creation of cholesterol in the liver, thus decreasing their overall level in the blood. They have been researched to be effective in their short-term goal of cholesterol reduction, but they are a life-long commitment of medication. Many question their side effects (myalgia, or muscle pain for some, low tolerance in others) contraindication in pregnancy, and a possible blinding effect to more overarching issues like poor nutrition or a sedentary lifestyle.
If the simplicity of taking a drug can distract us from making decisions that lead to longer term health, what happens when we choose not to use it any more? What habits are we grooming? Perhaps different lifestyle choices can be used collaboratively with statin drugs, to reduce dependence on Big Pharma and turn our attention back to creating our own healthy lifestyle. Enter: Exercise. Free, no negative side effects and many additional benefits.
Exercise and effects on Cholesterol:
We have a love-hate relationship with exercise (OMG why?!) More on this in another post, but for now let’s look at how exercise affects cholesterol levels. I’ll define exercise here as “movement to increase heart rate and respiration to meet increased activity-induced metabolic demands”.
Mechanisms are a bit murky, but it seems that exercise changes the size of LDL to make them less likely to stick on vessel walls, and increases transportation of LDL to the liver, expediting elimination. A metastudy suggests protective results of exercise are seen when folks exercise for at least 150 min/week, 5 X a week. This is a bare minimum. I suggest at least double that. Sitting is the new smoking - actually, don’t do either, they are both associated with increased risk of atherosclerosis.. (I recognize the irony of sitting to type this, I am looking forward to getting off my butt and going cross country skiing). Also, more intense exercise is more health-protective than moderate intensity, and both aerobic and resistance training are effective modalities in changing cholesterol levels.
“But I don’t have time to exercise…”
Actually, No - you don’t have time to be sick.
Though it’s much easier to take a pill than change your lifestyle and priorities, statins have a long list of inconvenient side effects (common ones are headache, muscle ache, flushing, drowsiness, dizziness, GI upset, rashes, and less common ones include hair loss, inflammation and sexual dysfunction). Plus there’s cost, medical appointments and insurance involved. Increased activity is free, available to everyone, and have very convenient side effects such as improved sleep, muscle tone, mood, bone mass, resilience, immunity, lower weight, blood pressure and stress levels, among many others. Reprioritizing to include more vigorous activity in your life is a choice that will have many long-lasting positive effects on your health.
From where I stand, if you are dealing with a diagnosis of dangerous cholesterol levels, statins are an effective and safe-enough-for-most quick fix. But it’s not the best long-term choice. Updating priorities and habits to add vigorous enjoyable movement to your life will have effects above and beyond cholesterol levels. And this is only one side of the coin - healthy food choices (a few quick tips above) are also very important.
Brainstorm about how to add more enjoyable vigorous playtime to your life to create your own joyful healthy lifestyle, minimize dependance on pharmaceuticals, and enjoy energetic spill-over of all the healthspan benefits statins cannot offer.